Our bodies are thriving habitats for other life-forms. Our guts, mouths, noses and skin support diverse communities of microbes that can be both good and bad for our health. But in recent years scientists have been finding microbes in an altogether more surprising place – in tumours.
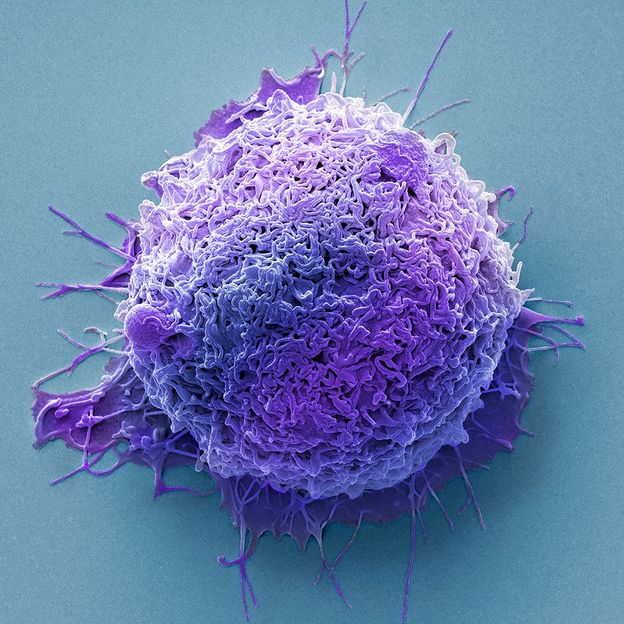
It is common to think of cancers as simply masses of a patient’s own cells that malfunction and grow uncontrollably. They are in fact communities of many different cell types, which is part of the reason why cancers are so hard to treat – it is difficult to target them without harming healthy tissue too.
But tumours also play host to a collection of cells from other life-forms entirely – bacteria and fungi. Some thrive in the environment around a tumour while others live inside the cancer cells themselves.
Until recently, however, the role that these microbes play in tumours has not been clearly understood. Now scientists are starting to unravel whether these tumour-associated microorganisms are accomplices that assist cancer cells as they develop or just unfortunate bystanders caught up in the tumour. And the answers could provide new approaches to treating and preventing cancers.
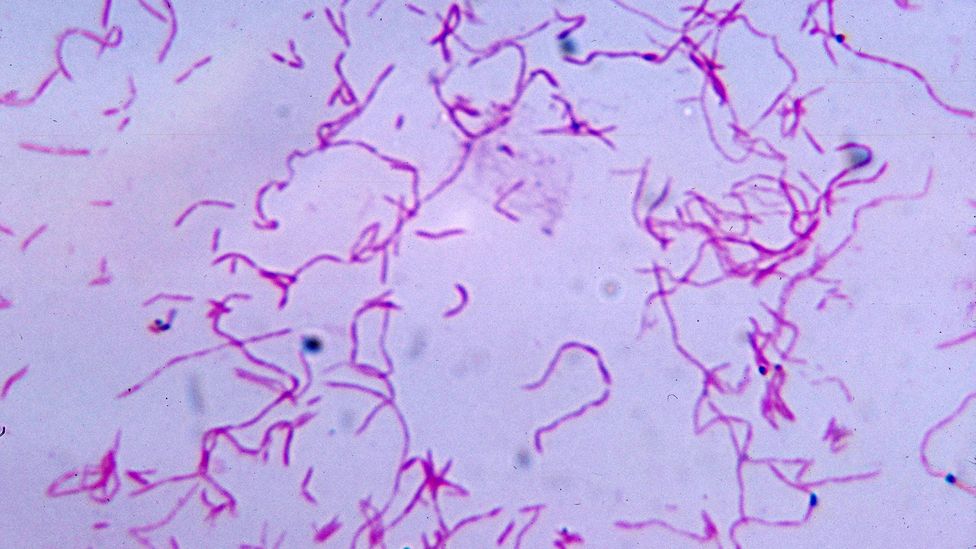
Fusobacterium nucleatum is commonly associated with the mouth, but is also found in many tumours (Credit: Alamy)
In a 2017 study Ravid Straussman, a cancer biologist at the Weizmann Institute of Science in Rehovot, Israel and his team showed that some bacteria living inside human pancreatic cancers can protect the tumours by inactivating a common chemotherapy drug. They found that one particular class of bacteria, known as Gammaproteobacteria, could break down gemcitabine: a drug used to treat a number of cancers including those found in the bladder, breast and pancreas. This helped the tumours become resistant to the drug. When the team injected mice with colon cancer with the bacteria, the mice’s cancers also became resistant to the drug. But when the researchers gave the mice an antibiotic alongside the chemotherapy drug, the resistance disappeared.
Further to these findings, research published in 2019 by a team at Tohoku University in Japan looked retrospectively at patients suffering from advanced cancers who were treated with either a chemotherapeutic drug alone and those who also received an antibiotic in addition to the chemotherapy in an attempt to prevent or treat an existing infection. They found that patients who were given an antibiotic had a better response to treatment. Although the study did not examine the amount of bacteria present in the cancer tissue of these patients, the researchers speculated that the antibiotics might have eliminated tumour-associated bacteria, which may have been interfering with the cancer treatment.
The studies offer a tantalising hint of what might be going on within tumours.
Straussman and his team are now hoping to build on these studies with a clinical trial involving patients with pancreatic cancer who failed their first line treatment. They will give patients an antibiotic known to act against Gammaproteobacteria, alongside a course of the chemotherapy drug gemcitabine, to see if the antibiotic improves their outcomes.
But bacteria might also play other roles in cancer beyond protecting tumours from drug treatment.
In 2020, Straussman’s team looked at more than 1,500 human tumours across seven different cancer types: breast, lung, ovary, pancreas, melanoma, bone and brain. They found all of the tumour types were invaded by bacteria, which lived inside the cancer cells and some of the immune cells. Different tumour types had distinct communities of bacteria.
“Each of these bacteria have adapted to the unique tumour microenvironment in which they live,“ says Straussman. “In lung cancer, we demonstrated how people who smoke have more bacteria which can degrade nicotine – which is a smoke-related metabolite. In bone cancers, we see bacteria which metabolise hydroxyproline, which is a metabolite enriched in bone tumours.”
In many cases it is still unclear whether the bacteria are helping the sufferer by keeping the cancer cells under control.
Bacteria found in some types of breast cancer, for example, can detoxify arsenate, a type of carcinogen known to increase the risk of breast cancer. Others can produce a chemical called mycothiol, which helps to reduce levels of harmful reactive oxygen molecules that can damage DNA.
There is growing evidence, however, that in some cases, the tumour-dwelling bacteria may actually be making cancers worse.
Some bacteria in breast tumours might make it easier for cancer cells to spread to other parts of the body
“More and more papers are coming out showing how they may be part of the carcinogenesis,” says Straussman. The bacteria may also be altering the ability of the immune system to target and destroy cancer cells, he adds. “But we are really scratching the surface here.” Much more needs to be done, he says, to study the effects that bacteria inside tumours have on the course of cancers.
There are already some clues. For example, a 2022 study by scientists in China suggests some bacteria in breast tumours might make it easier for cancer cells to spread to other parts of the body. The researchers found bacteria living inside breast tumour cells that were circulating in the blood of mice. These circulating cancer cells are shed from the primary tumour and can travel to other parts of the body, where they can metastasise and grow. However, as the tumour cells rattle around in the bloodstream, they are exposed to stress that causes some of them to break apart.
The Chinese researchers found that the microbes inside these mobile tumour cells seem to protect them from some of the stress they experience. They appear to do this by helping to reorganise internal cellular support structures known as the cytoskeleton so the cells are more robust. When the scientists eliminated these bacteria from the mice tumours, the tumours appeared to lose their ability to metastasise, although the primary breast cancer continued growing.
“There is growing evidence that specific microbes in the gut, the skin, and other mucosal organs, as well as in tumours, can either promote tumour growth and progression, or alternatively antagonise it,” says Douglas Hanahan, an oncologist at the Swiss Institute for Experimental Cancer Research in Lausanne, Switzerland, and the author of Hallmarks of Cancer: New Dimensions. However, the picture remains murky. “The landscape is very complicated, and while there are clues, there is no definitive clarity about who does what.”
Other studies looked at Fusobacterium nucleatum, an oral bacterium associated with gum disease, but might also be associated with a number of different cancers. It seems these bacteria can migrate from the mouth to colorectal cancer cell through the bloodstream. Each bacterium carries specific particles on its surface that bind to the surface of cancer cells, allowing it to colonise them.
Once in place, the bacteria can accelerate the growth and spread of tumours, by hampering the immune system’s ability to kill cancer cells. A protein produced by Fusobacterium nucleatum binds to a molecular control mechanism on the surfaces of human natural killer cells and T cells, which are both key parts of the immune system’s defences against tumours. This binding inhibits the cells’ ability to destroy cancer cells. The bacteria also deploy a molecular arsenal that makes cancer cells more resistant to chemotherapy.
Furthermore, Fusobacterium nucleatum‘s DNA has been found in human breast cancer samples. This suggests it also affects tumours elsewhere in the body. In one study, when the bacteria were introduced to mice with breast cancer, it accelerated the progression and spread of the disease. Giving the mice antibiotics prevented this.
It may seem tempting to include antibiotics in cancer therapies, but it is not as simple as that. Many of the microbes in our bodies are benign or even beneficial, so a brute-force antibiotic treatment could cause more harm than good, says Hanahan.
Instead, researchers must try to unravel the full complexity of the tumour-associated microbiome. Entire communities of microbes can be found within tumours, and they support each other in unexpected ways.
Many of the bacteria associated with colorectal cancers can work together to make the patient’s condition worse (Credit: Getty Images)
One such example revolves around the primary chemotherapeutic drug used to treat patients with colorectal cancer, 5-fluorouracil (5-FU). It seems to inhibit the growth of the troublesome Fusobacterium nucleatum. However, certain strains of Escherichia coli – commonbacteria found in the gut – render the drug inactive.
Researchers led by Susan Bullman, a cancer microbiologist at the Fred Hutchinson Cancer Centre in Seattle, US, found that the inactive form of 5-FU no longer inhibited cancer in laboratory cell cultures. It also no longer prevented Fusobacterium nucleatum’s growth. This led Bullman and her colleagues to hypothesise that patients who do not respond to 5-FU treatment may carry bacteria that inactivate the drug. These bacteria may allow Fusobacterium nucleatum the chance to flourish, making the patients’ conditions worse.
You might also be interested in:
- How exercise can give your microbiome a boost
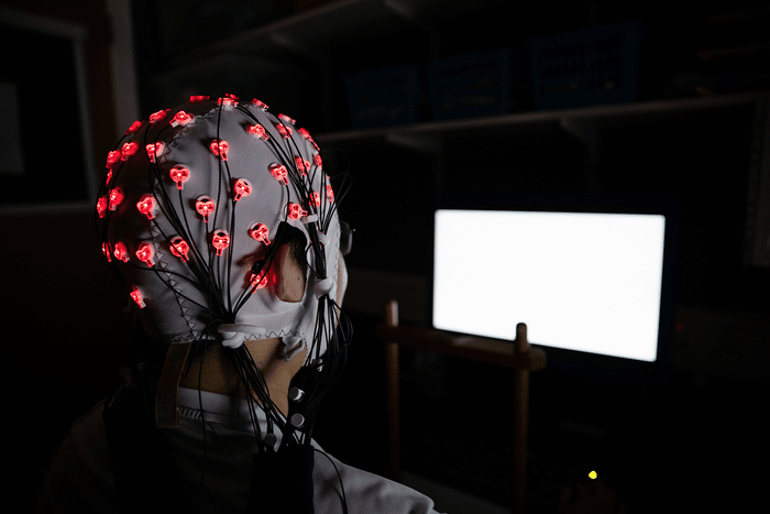
- The bacteria controlling your brain
- The 77-million-year-old cancers
At least 33 different types of cancer have now been found to have colonies of bacteria associated with them, thanks to techniques developed at the University of California, San Diego, that look for their DNA. The researchers believe the techniques could also be used to develop new ways of diagnosing cancer, by looking for the DNA from distinct tumour-associated bacteria in a patient’s blood.
The team behind this study joined forces with Ravid Straussman for a 2022 study that revealed another type of microbe – fungi – living in cancer. They found fungi in 35 different types of cancer, many of which housed distinct combinations of species.
“We found that tumours which have more bacteria also have more fungi, and ones with less bacteria have less fungi,” says Straussman. “We can only hypothesise at this point that some tumours are more restrictive for the presence of microbes in them and some are more permissive.”
Just as with bacteria, some of these fungi appear to be manipulating the immune system in the tumour’s favour. The fungus Malassezia globosa has been found to speed up the development of one form of pancreatic cancer. The same fungi have also been found in breast cancer patients who tend to have shorter overall survival, according to work by Straussman and his University of California, San Diego colleagues. Other research has found that some fungi present in pancreatic cancers hijack parts of the immune system to promote tumour growth.
A 2022 study also showed that stomach cancers rich in Candida fungi show increased expression of tumour genes that promote inflammation and that colon tumours rich in Candida DNA are more likely to be metastatic. This “might be because increased numbers in Candida may be associated with loss of gut epithelial barrier [the cells lining the gut],” says Iliyan Iliev, a microbiologist at Cornell University, whose team conducted the research.
Despite the rapid pace of these findings, many questions still remain about the relationship between tumours and the microbes that live in them. Do the microbes play a role in the development of the tumour in the first place? Or are they simply opportunistic residents that have adapted to protect their cancerous home when they find one? And can this microbe community be harnessed to help us in our fight against cancers?
In years to come, targeting tumour microbes may become as important as going after the cancer cells themselves, leading to earlier diagnoses and even new treatments. But that work has only just begun.
Source: BBC.COM